artificial heart
Introduction
 device that maintains blood circulation and oxygenation in the human body for varying periods of time. The two main types of artificial hearts are the heart-lung machine and the mechanical heart.
device that maintains blood circulation and oxygenation in the human body for varying periods of time. The two main types of artificial hearts are the heart-lung machine and the mechanical heart.Heart-lung machine (heart–lung machine)
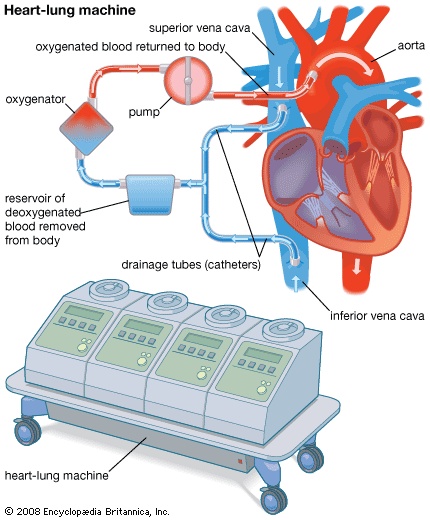 The heart-lung machine is a mechanical pump that maintains a patient's blood circulation and oxygenation during heart surgery by diverting blood from the venous system, directing it through tubing into an artificial lung (oxygenator), and returning it to the body. The oxygenator removes carbon dioxide and adds oxygen to the blood that is pumped into the arterial system. The blood pumped back into the patient's arteries is sufficient to maintain life at even the most distant parts of the body as well as in those organs with the greatest requirements (e.g., brain, kidneys, and liver). To do this, up to 5 litres (1.3 gallons) or more of blood must be pumped each minute. While the heart is relieved of its pumping duties, it can be stopped, and the surgeon can perform open-heart surgery that may include valve repair or replacement, repair of defects inside the heart, or revascularization of blocked arteries.
The heart-lung machine is a mechanical pump that maintains a patient's blood circulation and oxygenation during heart surgery by diverting blood from the venous system, directing it through tubing into an artificial lung (oxygenator), and returning it to the body. The oxygenator removes carbon dioxide and adds oxygen to the blood that is pumped into the arterial system. The blood pumped back into the patient's arteries is sufficient to maintain life at even the most distant parts of the body as well as in those organs with the greatest requirements (e.g., brain, kidneys, and liver). To do this, up to 5 litres (1.3 gallons) or more of blood must be pumped each minute. While the heart is relieved of its pumping duties, it can be stopped, and the surgeon can perform open-heart surgery that may include valve repair or replacement, repair of defects inside the heart, or revascularization of blocked arteries.The first successful clinical use of a heart-lung machine was reported by American surgeon John H. Gibbon, Jr., in 1953. During this operation for the surgical closure of an atrial septal defect, cardiopulmonary bypass was achieved by a machine equipped with an oxygenator developed by Gibbon and a roller pump developed in 1932 by American surgeon Michael E. DeBakey. Since then, heart-lung machines have been greatly improved with smaller and more-efficient oxygenators, allowing them to be used not only in adults but also in children and even newborn infants.
Mechanical hearts
 Mechanical hearts, which include total artificial hearts and ventricular assist devices (VADs), are machines that are capable of replacing or assisting the pumping action of the heart for prolonged periods without causing excessive damage to the blood components. Implantation of a total artificial heart requires removal of both of the patient's ventricles (lower chambers). However, with the use of a VAD to support either the right or the left ventricle, the entire heart remains in the body. Mechanical hearts are implanted only after maximal medical management has failed. They may be used for cardiac resuscitation after cardiac arrest, for recovery from cardiogenic shock after heart surgery, and in some patients with chronic heart failure who are waiting for a heart transplant. Occasionally, mechanical hearts have been used as a permanent support in patients who do not qualify for a heart transplant or as a bridge to recovery of the patient's own diseased heart. The goal is to provide a safe, effective system that allows the recipient to move about freely, thus improving the quality of life. Some recipients of VADs have lived several years and have returned to work and normal physical activities.
Mechanical hearts, which include total artificial hearts and ventricular assist devices (VADs), are machines that are capable of replacing or assisting the pumping action of the heart for prolonged periods without causing excessive damage to the blood components. Implantation of a total artificial heart requires removal of both of the patient's ventricles (lower chambers). However, with the use of a VAD to support either the right or the left ventricle, the entire heart remains in the body. Mechanical hearts are implanted only after maximal medical management has failed. They may be used for cardiac resuscitation after cardiac arrest, for recovery from cardiogenic shock after heart surgery, and in some patients with chronic heart failure who are waiting for a heart transplant. Occasionally, mechanical hearts have been used as a permanent support in patients who do not qualify for a heart transplant or as a bridge to recovery of the patient's own diseased heart. The goal is to provide a safe, effective system that allows the recipient to move about freely, thus improving the quality of life. Some recipients of VADs have lived several years and have returned to work and normal physical activities.A left VAD pumps oxygenated blood from the left ventricle to the aorta. The pumping part of the device is implanted in the left upper abdomen or left side of the chest. A tube from the pump exits the skin and connects to a controller that regulates the function of the pump and to a power source. Pneumatic (pneumatic device) devices have membranes or sacs that are moved by air pressure to pump the blood, while electrical devices use electromechanical systems for power. Electrical devices are being developed that are totally implantable and do not require a tube exiting the skin; with these devices, power to the pump is transmitted between external and internal batteries through the intact skin.
Most mechanical hearts incorporate various centrifugal pumps (pump), paracorporeal pulsatile pumps, cardiopulmonary bypass (CPB) pumps, and the intra-aortic balloon pump (IABP). These pumps generate a pulsatile blood flow and pressure similar to those of the natural heart. Smaller devices known as axial flow pumps, on the other hand, generate continuous blood flow by a jet-engine type of technology. An experienced surgical team chooses the particular device to be implanted by assessing the patient's size, the amount of support the heart requires, and the expected duration of support.
The first successful use of a mechanical heart in a human was performed by Michael E. DeBakey (DeBakey, Michael) in 1966. After surgery to replace the patient's aorta and mitral valve, a left VAD was installed, making it possible to wean the patient from the heart-lung machine; after 10 days of pump flow from the VAD, the heart recovered, and the VAD was removed. During the 1970s synthetic materials were developed that greatly aided the development of permanent artificial hearts. One such device, designed by American physician Robert K. Jarvik, was surgically implanted into a patient by American surgeon William C. DeVries in 1982. The aluminum and plastic device, called the Jarvik-7 for its inventor, replaced the patient's two ventricles. Two rubber diaphragms, designed to mimic the pumping action of the natural heart, were kept beating by an external compressor that was connected to the implant by hoses. This first recipient survived 112 days and died as a result of various physical complications caused by the implant. Subsequent patients fared little better or even worse, so that use of the Jarvik-7 was stopped. In 2001 a team of American surgeons implanted the first completely self-contained artificial heart, called the AbioCor artificial heart. The patient survived 151 days.
In 2008 a fully functional artificial heart was developed by Carmat, a French company founded by cardiologist Alain Carpentier. The device was covered with a specially designed biosynthetic material to prevent the development of blood clots and to reduce the likelihood of immune rejection—problems associated with the AbioCor and Jarvik-7 artificial hearts. The Carmat heart also utilized sensors to regulate blood flow and heartbeat. Plans to test the heart first in calves and sheep and later in humans with terminal heart failure were being developed.
- Nicodemus, The Elder Tessin
- Nicodemus The Hagiorite, Saint
- Nicodemus, The Younger Tessin
- Nicola Antonio Zingarelli
- Nicolaas Beets
- Nicolaas Bloembergen
- Nicolae Ceaușescu
- Nicolae Davidescu
- Nicolae Iorga
- Nicolae Milescu
- Nicolae Rădescu
- Nicolaes Maes
- Nicolaes Pietersz Berchem
- Nicolae Titulescu
- Nicola Fabrizi
- Nicolai Abraham Abildgaard
- Nicolai, Friedrich
- Nicolai Hartmann
- Nicolai, Otto
- Nicola Pisano
- Nicola Porpora
- Nicola Sabbatini
- Nicola Salvi
- Nicolas Appert
- Nicolas Boileau